Alzheimer’s or Dementia & Pain: What Caregivers Need to Know
When someone you love has dementia, it’s not always easy to tell if they’re hurting. Dementia itself doesn’t cause pain—but many people living with it have other health issues like arthritis, diabetes, or dental problems that do. The tricky part is, your loved one may not recognize the pain, or may not be able to explain what’s wrong.
As a caregiver, you often have to play detective—watching for clues in their face, movements, or behaviors. Unrecognized pain is one of the biggest hidden causes of restlessness, agitation, or sudden changes in mood.
The good news? There are tools and strategies you can use to spot pain early, bring comfort, and share helpful information with your doctor. In this article, we’ll cover how to recognize the signs of pain in dementia, what treatments can help, and why managing pain is such an important part of quality care.

Understanding Types of Pain
Pain is your body’s alarm system. It tells you something’s wrong. It can be:
- Acute pain – New, short-term (like a cut, bruise, or toothache).
- Chronic pain – Lasting longer than 3 months (like arthritis, back pain, or cancer).
People describe pain in different ways: aching, burning, cramping, dull, sharp, throbbing. These clues can help doctors figure out the cause and best treatment.

Common Causes of Pain in Alzheimer’s or Dementia
People with dementia often live with other health conditions that bring pain, such as:
- Arthritis and joint stiffness
- Back pain
- Constipation
- Diabetic neuropathy (tingling or burning in feet/hands)
- Pressure sores from sitting or lying too long
- Tooth pain or poorly fitting dentures
Your Roadmap Through Alzheimer's & Dementia Care
✨ The more you understand dementia, the more patience you’ll have for the journey.
That’s why I created the Understanding Dementia Course — to help you gain both clarity and compassion.

Recognizing Pain In Alzheimer’s or Dementia
If your loved one can’t tell you what hurts, watch for nonverbal signs. Some caregivers use pain assessment tools like:
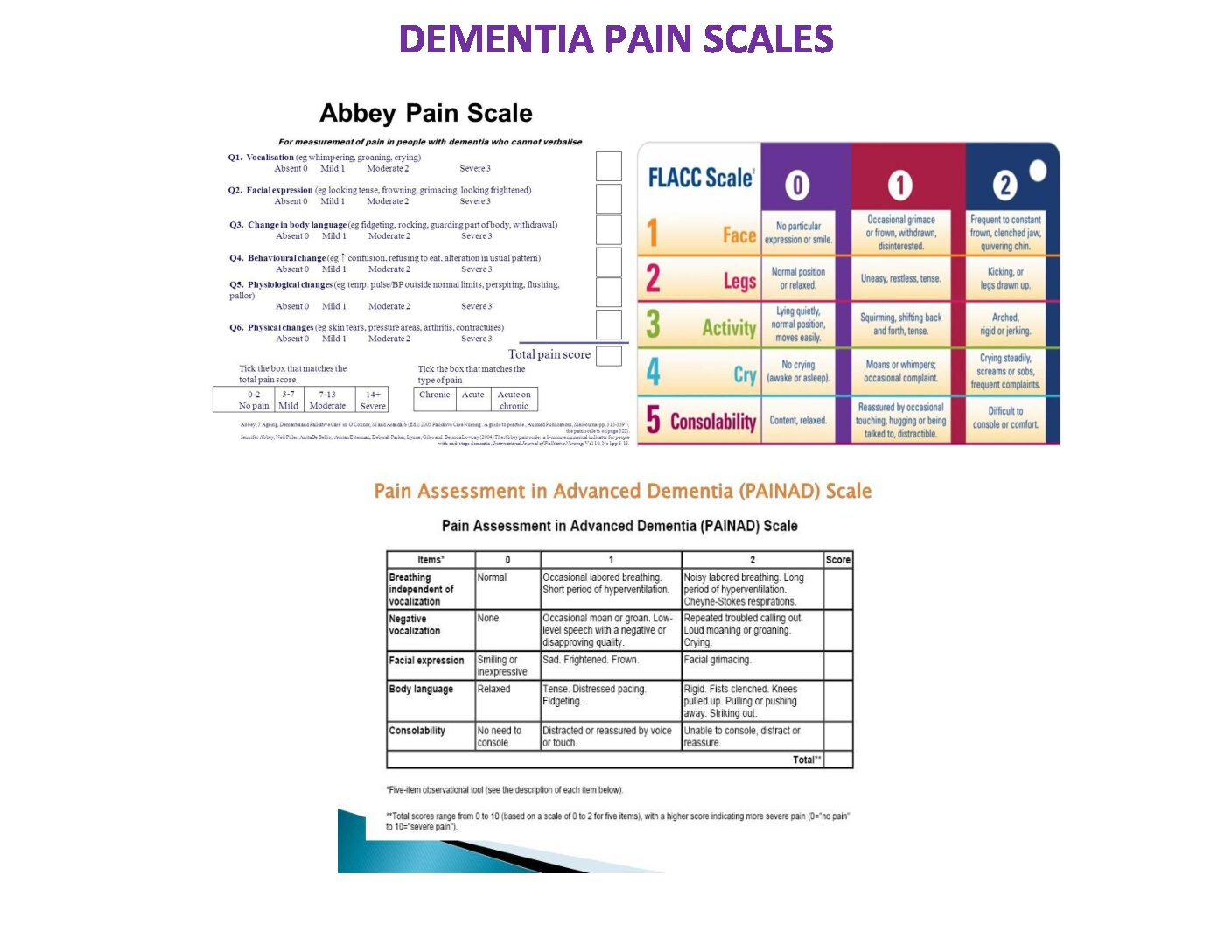
PAINAD (Pain Assessment in Advanced Dementia) Scale:
Looks at breathing, facial expressions, body language, sounds, and how easily they can be comforted.
Focuses on facial changes, body movements, and behavior shifts.
Uses pictures of faces ranging from happy to very distressed.
Scores pain by watching face, legs, activity, crying, and how easily consoled.
What to Look For
When you’re trying to figure out if your loved one has pain, pay attention to:
- Location: Do they grab a body part or avoid using it?
- Timing: Does it seem worse at night, after meals, or during activity?
- Severity: Watch their expressions, movements, and behaviors to gauge if it’s mild, moderate, or severe.
- Triggers & Relief: What makes it worse or better (position changes, rest, movement, medication)?

Treating Pain in Alzheimer’s or Dementia
Medications
Tylenol (Acetaminophen): A First Step for Pain Relief
For most people with dementia, Tylenol (acetaminophen) is the safest and most effective first choice for everyday pain—unless their doctor advises against it.
Here’s something many caregivers don’t realize: Tylenol works best when it’s given on a schedule, not just when your loved one looks uncomfortable. If you wait until the pain is already strong, it can take much longer to bring relief.
Think of it like a “comfort cushion.” When you give the next dose before the last one wears off, you keep the pain level steady and prevent those sharp spikes of discomfort. This doesn’t mean giving it too often or more than prescribed—it means following a safe, doctor-approved routine (like every 6–8 hours, depending on instructions).
💡 Caregiver Tip:
-
Ask your doctor what a safe schedule looks like for your loved one.
-
If it’s approved, giving Tylenol 2–3 times a day—especially one dose at bedtime—can help your loved one stay more comfortable, move more easily, and even sleep better through the night.
-
Always check for maximum daily limits (usually no more than 3,000 mg in older adults, unless the doctor advises otherwise).
By keeping pain under control, you’re not just easing discomfort—you’re also helping prevent restlessness, sleep problems, and agitation that can come when pain sneaks back in.
Nsaids (Nonsteroidal anti-inflammatory drugs like ibuprofen) may help but carry risks for stomach, kidney, and heart issues—so only use short-term and under doctor guidance.
Opioids/Narcotics can help with severe pain but may worsen confusion or cause delirium. Always monitor closely and update the doctor.

Non-Medication Options
- Gentle exercise or stretching
- Massage or warm packs for sore muscles
- Cold packs for swelling or injury
- Aromatherapy or calming music
- Distraction (puzzles, TV, or pleasant activities)
- Relaxation techniques like deep breathing
💡 Caregiver Tip:
For most people with arthritis or joint pain, keeping up a regular schedule, including physical activity, will help them feel better. Remember, sitting or lying for long periods of pain can cause discomfort.
Discover the Key to Understanding Alzheimer's & Dementia
💡 Alzheimer’s & Dementia can feel overwhelming, but when you understand what’s happening, patience becomes easier.
The Understanding-Dementia Course gives you the tools to prepare, cope, and care with more peace.

Why Pain Management Matters
Untreated pain can impact sleep, appetite, mobility, quality of life, and behavior. It can even lead to increased confusion or difficult behaviors. If your loved one seems agitated, always consider whether pain might be the cause and try different ways to bring relief.
Take time to watch your loved one for at least 5 minutes at different points in the day. Morning, afternoon, and evening can each reveal different clues. One of the best times to spot pain is during dressing or undressing. That’s because these moments involve bending, lifting arms, sitting, standing, and sometimes balancing. If pain is present, it often shows up here in ways you can see.
Here’s what to look for:
-
Facial expressions: grimacing, wincing, or frowning during movement.
-
Body movements: guarding a sore spot, moving stiffly, or resisting certain motions.
-
Sounds: sighing, groaning, gasping, or crying out with movement.
-
Avoidance: refusing to raise arms for a shirt, keeping legs stiff, or not wanting to stand.
-
Behavior changes: irritability, snapping, or refusing care—sometimes it’s pain, not “just behavior.”
Untreated pain doesn’t just cause discomfort—it can show up as agitation, aggression, pacing, or withdrawal. These “challenging behaviors” may actually be pain talking.
That’s why tracking pain is so important. Write down what you see during daily routines like dressing, walking, or sitting down. Do they wince? Hold onto furniture? Grimace when lifting an arm? Those are valuable clues to share with their doctor. Over time, your notes can reveal patterns, leading to better treatment and more comfort for your loved one.
Essential Steps for Managing Pain in Dementia Care
Once you’ve learned how to spot the signs of pain, the next step is knowing how to respond. Here’s a simple caregiver roadmap:
- Look for Signs of Pain
Observe your loved one throughout the day, especially during daily routines like dressing, walking, or eating. Use pain scales (like PAINAD or FLACC) if your loved one cannot describe their pain. - Try Comfort Measures First
Before reaching for medicine, try small changes: adjusting their position, offering a warm pack, a gentle massage, calming music, or distraction with an activity they enjoy. - Use Tylenol (if approved by the doctor)
Tylenol (acetaminophen) is usually the first choice for ongoing pain. Remember, it works best on a schedule—not just “as needed.” Giving the next dose before the last one wears off helps keep pain under control and prevents sudden spikes of discomfort. Always follow the doctor’s dosing instructions. - Reassess for Relief
Watch your loved one closely after an intervention. Do they seem calmer? Are they moving more easily? A change in mood, expression, or activity level can signal that the pain is better managed. - Keep Track
Write down what you observed, what you tried, and how well it worked. Notes on pain patterns—like “worse in the evening” or “grimaces when lifting arms”—help the doctor make better treatment decisions. - Call the Doctor if Needed
If pain is not improving, if you notice new signs of discomfort, or if you’re unsure, contact your doctor. They may recommend different treatments, therapies, or medication adjustments. - Share What You’ve Learned
Bring your notes (from a notebook or an app like Alzlog) to appointments. This turns vague descriptions like “She seems uncomfortable” into clear, useful information the doctor can act on.
💛 Remember: Managing pain isn’t just about comfort—it can improve sleep, appetite, mood, and even reduce challenging behaviors. Every small step you take helps your loved one feel safer and more at peace.
These Dementia Pain videos are very helpful and will help you better understand Dementia and pain.
please take a few minutes to watch them.
Final Thoughts: Easing Pain, Bringing Comfort
Caring for someone with dementia is never easy, especially when pain enters the picture. Unrecognized pain can steal sleep, cause agitation, and make daily life harder for both of you. But when you learn to spot the signs, track what you see, and share it with the doctor, you give your loved one the best chance at comfort and peace.
Remember—you don’t have to guess alone. Tools like the Caregiver’s Notebook and the Alzlog app can make it easier to keep track of pain, behaviors, and changes over time. These notes become a powerful resource for you and your loved one’s medical team, helping ensure their pain is taken seriously and treated effectively.
💛 Your efforts matter. By being their advocate, detective, and comforter, you’re making a real difference in their quality of life.
Hi, I’m Larea, a Registered Nurse, Faith Community Nurse, and Certified in Dementia Care with 30 years of experience supporting families living with Alzheimer’s and other dementias. Both of my parents have Dementia, so I understand the journey personally as well as professionally. My heart is in helping family caregivers feel supported, prepared, and confident every step of the way.







0 Comments