WHAT IS DEMENTIA PAIN?
When I refer to Dementia pain, I mean someone with Dementia who has pain somewhere in their body and may or may not be able to communicate that pain to a caregiver.
Dementia by itself is not painful. Unfortunately, most people with Dementia are elderly and have other medical conditions that may cause pain.
Pain is simply your body’s way of letting you know something is wrong.
It can also be described as an unpleasant sensation ranging from mild discomfort to agony.

Acute vs. Chronic
Pain is usually referred to as either acute or chronic. Acute pain is new pain and lasts less than three months. Acute pain may be related to an injury such as a cut or toothache. Chronic pain is ongoing and lasts longer than three months. Examples of chronic pain include arthritis, back pain, or cancer pain.
Pain Descriptors
There are so many words to describe different types of pain. The descriptions help your doctor determine the source of the pain and the appropriate treatment. Here are a few terms often used to describe pain.
- Aching
- Agonizing
- Burning
- Comes and goes
- Constant
- Cramping
- Dull
- Fearful
- Gnawing
- Heavy
- Hot or burning
- Pinching
- Prickly
- Sharp
- Shooting
- Sickening
- Splitting
- Stabbing
- Stinging
- Tender
- Throbbing
- Tingle
Shelter of Calm:
Your Guide Through Dementia's Storm!
Is Dementia's chaos stealing your peace?
We're here to restore the calm, empowering you to confidently face each challenge.
Take the first step towards transformation now.


What kind of pain do dementia patients have?
Many people with Dementia also have a comorbidity that causes pain. Comorbid simply means the presence of two or more diseases or medical conditions. An example would be your loved one who has Dementia, but also Diabetes. Diabetes can lead to neuropathy, a tingling/burning/pain in the legs, feet, and hands.

People with Dementia are at the same risk of pain as everyone else.
Potential causes of pain are the same for people with Dementia as for everyone else. They can include:
Arthritis
Back Pain
Constipation (gas/cramping/spasms)
Foot pain (shoes rubbing)
Headaches
Infections
Neuropathy feet/hands
Old injuries
Pressure injury (sitting in one position too long)
Toothaches/Denture pain
Unknown injuries
Urinary Tract Infection (UTI)
The difference is they may be unable to recognize the pain or ask for help. This is why it is so essential Dementia caregivers learn how to identify the signs of pain and track it.
Recognizing Dementia Pain
How can you tell if a dementia patient is in pain? This can be tricky sometimes. As a dementia caregiver, you must learn how to become a pain detective. Fortunately, there are several pain scales that can help you assess the pain in your loved one.
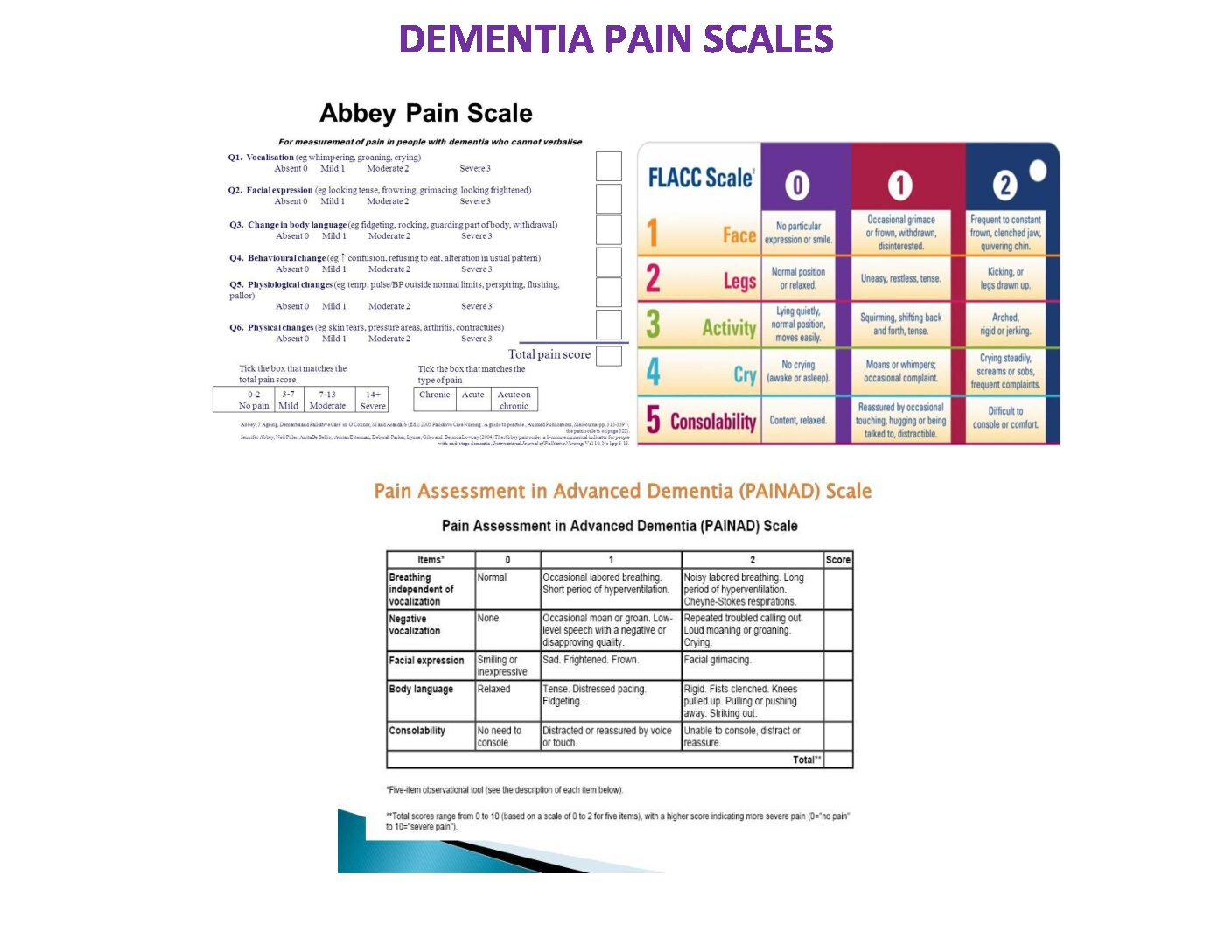
PAINAD (Pain Assessment in Advanced Dementia) Scale:
- What it Measures: Specifically designed for advanced dementia patients who may have difficulty communicating pain.
- How it Works: It looks at five categories: breathing, negative vocalization, facial expression, body language, and consolability. Each category is given a score, and the total helps determine the presence and intensity of pain. Each area is scored, with possible total scores of 0 (no pain) to 10 (severe pain).
- What it Measures: Developed for people with dementia, it assesses pain based on facial expression, vocalization, change in body language, and behavioral cues.
- How it Works: It looks at various indicators and assigns a score to each, giving a comprehensive picture of the person’s pain experience.
- What it Measures: This one is pretty straightforward. It uses a series of faces with different expressions to help the person express their pain level.
- How it Works: The individual points to the face that best represents their pain, ranging from a happy face (no pain) to a sad or distressed face (more pain).
- What it Measures: FLACC stands for Face, Legs, Activity, Cry, and Consolability. It’s mainly used for non-verbal individuals, like those with dementia.
- How it Works: Each category is scored from 0 to 2, and the total helps gauge pain severity. It looks at facial expressions, leg movements, activity level, crying, and how easy it is to console them
ASSESSING DEMENTIA PAIN
You must help your doctor determine if your family member has any pain. Then, the better picture you can paint for him, the more appropriately he can treat any pain. The following information will help you paint that picture.
Location: Ask if the pain radiates from one position to another: i.e.…, from the back, down the leg, from the abdomen to back. If they are unable to tell you, watch for signs of pain.
Quality: If possible, please describe what it feels like in the family members’ words. How pain is described is often a clue to its origin.
Timing: In relationship to events, meals, bathing or change in position. Does it begin suddenly or come on gradually? Does it seem worse at night or in the morning?
Severity: Describe what it is now and at its worst. Determine whether the pain is mild, moderate, severe, or severe. Watch for non-verbal signs of pain, especially in someone who cannot describe the pain’s severity. Use your judgment to rate severity when your family member can not. Factors that worsen or improve pain? Medication, relaxation, movement, breathing, position, bracing, sitting, lying down or one side, etc.….

How to treat Dementia pain
Medications for treating Dementia pain.
Tylenol/Paracetamol is still the preferred pain medication for those with Dementia, unless contraindicated. One of the biggest problems with pain management in those with Dementia is that the medicine is not given routinely. Especially in facilities, if it isn’t scheduled, it usually isn’t given since they can’t ask for it.
It is recommended to give it scheduled to help keep the pain controlled around the clock.
I have found a Tylenol 2 or 3 times a day can help with Dementia pain, especially a dose at bedtime. It can help them sleep better if they are having discomfort at night. Ask your doctor if it is OK to start your family member with Dementia on a scheduled routine of Tylenol.
Nsaids such as Ibuprofen have serious side effects and should not be used for longer than two weeks without your doctor’s approval.
Opioids/Narcotics can also have side effects, including increased confusion and possible Delirium. If using, go slow and track the results and side effects. Make sure you keep your doctor updated.

Non-pharmacological pain treatment is how the medical world describes pain treatments that don’t involve medicines. These are usually tried first or used with pain medicine. Non-pharmacological pain interventions include:
Activity therapy
Aromatherapy
Distraction
Gentle exercise and stretching
Heat or cold packs
Massage
Music therapy
Relaxation
For most people with arthritis or joint pain, keeping up a regular schedule, including physical activity, will help them feel better. Remember, sitting or lying for long periods of pain can cause discomfort.
Consequences of untreated Dementia pain: Pain can affect all areas of their life, including activity, function, sleep, mobility, appetite, quality of life, agitation, confusion, and increased difficulty in providing care.
Watch your loved one for at least 5 minutes at different times during the day to see if you can see any signs of pain. One of the best times to determine if someone has pain is while getting dressed or undressed. When they walk, do they hang on to furniture or the wall? It may be for added balance but can also be pain-related.
Watch their facial expressions. Do they grimace? Do they pull away?
Uncontrolled pain is often the root cause behind challenging behaviors. So if your loved one has behaviors, put on your detective hat and look for any signs of pain. Then, try different pain interventions and track the results to see if the behaviors improve.
If you are a Dementia caregiver, whether at home or in a facility, you must learn the following steps.
- Recognize the signs of pain – use a pain scale (Painad preferred)
- Try to ease the pain without medicine. If there is no relief, go to the next step
- Try Tylenol if ok with your Doctor
- Re-assess if your intervention helped
- Keep track of the pain, interventions, relief
- If there is no relief, call the Doctor
- If pain is relieved, share the information you collected with your Doctor and ask him about scheduling Tylenol
If you don’t currently have a pain tracking system, please take a few minutes and check out The Caregivers Notebook. It was designed to help you track pain and other information your doctor needs to know.
These Dementia Pain videos are very helpful and will help you better understand Dementia and pain.
please take a few minutes and watch them.
You can find more information on Dementia pain management at the IASP (International Association for the Study of Pain)
The Dementia Caregiver Blog Library
Activities, Advanced Directives, Agitation, Apathy, Approach, Apps for Caregivers, Basic Caregiving, Bathing, Bathroom Safety, Caregiver Burnout, Caregiver Compassion, Caregiver Emotions, Caregiver Help, Caregiver Loneliness, Caregiver Support, Cold & Flu Season, Communication Challenges, Dehydration, Dementia Complications, Dementia Doctors, Dementia Safety Home, Dementia Types, Dementia-Friendly, Dressing Issues, Driving Safety, Eating Problems, Fall Prevention, Family Help, Finances, Guns & Dementia, Harm Prevention, Healthcare, Help at Home, Hiding Dementia, Holidays, Hospice, Hospital Stay, In-Between Stage, Kitchen Safety, Laughter, Legal Healthcare, Marijuana use, Medication Tips, Music, Nutrition, Pain, Patience, Poop Problems, Relationships, Reminiscing, Routine, Safety, Sense of Purpose, Shadowing, Sleep Issues, Stages of Dementia, Sundowning, Television, Time Travel, Traveling, Toileting, Wandering
Exploring Caregiving Tools & Resources? Don't Forget to Check Out My Resource Page! 🌟

Hi, I’m Larea, a Certified Dementia Specialist and Registered Nurse with 30 years of hands-on experience helping dementia patients in various settings, from hospitals to nursing homes and hospice. Drawing on personal experiences with my family members and patients over the years, I’m here to help guide you on your caregiving journey.


0 Comments