The Alzheimer’s Approach
Alzheimer’s Disease is not just memory loss
Their brain is failing, and everything is changing for them! It affects language, reasoning, attention, perception, abstract thinking, judgment, motor skills, and memory. This knowledge should help you realize why it is crucial that you understand the changes and learn how to approach them correctly. In addition, the correct Alzheimer’s approach will lead to trust and cooperation.
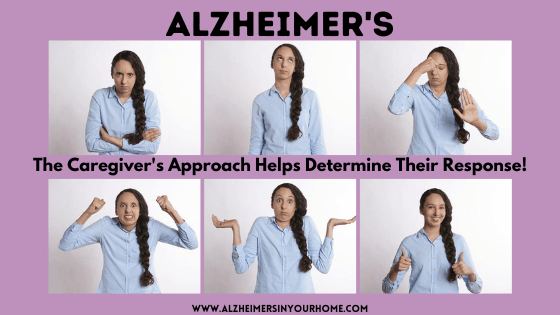
The wrong Alzheimer’s approach will lead to fight, flight, or fright.
When a person feels a threat of any kind (such as when they are startled), their body reacts. Generally, they react in one of those three ways.
Learning the correct Alzheimer’s approach for someone with Alzheimer’s or another form of Dementia increases their trust and comfort level with you. Which, in turn, increases the likelihood of their cooperation. I have taught hundreds of CNAs about the approach during my nursing career.
It is important to realize, this truly does make a difference.



The correct Alzheimer’s approach has six main components.
- Approach slowly
- Stand to the side
- Eye level
- Soft voice
- Call them by their first name
- Offer your hand
Approach from the front and slowly instead of the side where they can’t see you coming
Firstly, when you approach someone with Dementia, walk slowly and directly in front of them.
Walk as if you have all the time in the world to get there. They will see you coming and be able to process someone coming toward them if you walk slowly. Always avoid startling them (remember they have a narrowed vision field now).
Secondly, standing to the side while you are talking to them does not feel as threatening as someone standing before them.
To help gain their trust, you need to be at the same eye level. For example, squat down to their level if they are sitting in a chair. Don’t lean over to them. That position feels threatening. If you squat in front of them, they will feel they have control over the situation.
Thirdly, speak in a soft, calm voice.
Your tone should be friendly. Imagine yourself talking to a lost, scared animal stuck, and you need to gain trust to help them. But remember, there is a fine line between talking to an adult with Dementia and a child. You will demean them if you speak to them as if they are a child. Demeaning someone with Dementia usually leads to increasing agitation.
Fourthly, call them by their first name.
I learned this many, many years ago. The nursing school taught us to call everyone Mr. or Mrs. out of respect for that person. With Alzheimer’s or other Dementia people, using their first name implies you know them. They may not recognize you, but they will feel a connection to you. Therefore, they are much more likely to respond when you call them by their first name.
Lastly, offer your hand.
If you want them to complete a task, offer your hand. By taking your hand, it becomes their choice to go with you. People are more likely to cooperate when they feel it is their choice
The correct Alzheimer’s Approach to tasks
- There are two ways to complete a task.
- The task-centered approach is when the caregiver is focused on completing the task. An example would be bath time at 8:00, and the goal is to complete the bath at this time.
- or
- The patient-centered approach is when the caregiver works the task around the patient. An example would be the patient has always taken their shower in the morning after breakfast, and they adjust the bathing care to fit their usual routine.
-
Connect with them first before you attempt any/every task.
- Once you have made a connection, you will find them to be more cooperative. Offer a friendly comment. Find a common ground topic to talk about. Maybe previous work, family, church, sports, or perhaps their hometown.
- Here are the questions I always ask when meeting an elderly patient for the first time.
- I ask them if they are retired. It doesn’t matter if they are 100. I still ask this question. It helps me find out what they did.
- My next question is, are there grandchildren? This leads to talking about all their family.
- I ask if they are religious and if they attend a local church. Religious people often like to talk about their beliefs.
- I want to get them talking about their town. I ask if they are from this city. Often, they are not, which will lead to some reminiscing.
- Reminiscing is a valuable tool to use with someone with Alzheimer’s Disease since they lose their newest memories first. They are often more comfortable talking about events from the past.
Shelter of Calm:
Your Guide Through Dementia's Storm!
Is Dementia's chaos stealing your peace?
We're here to restore the calm, empowering you to confidently face each challenge.
Take the first step towards transformation now.

Completing a Dreaded Task using the Alzheimer’s Approach
If you want them to complete a task they are not fond of, it helps to change your wording.
Don’t throw out task-driven words right away, try using another word instead. The most common task words they don’t respond well to are bath, shower, and toileting. Remember, these are tasks they did their entire life privately. It feels intrusive when you are asking them to do something with you. It is important you realize this feels unnatural to them.
You know your task goal, but it is often best not to say it to them. Instead, you can use a transition phrase to get them up and to move, such as:
Let’s go for a walk
Can you help me with something?
It’s about time to…
When you enter the room where you want to complete the task, it works best if you ease into it in small steps. Such as let’s go ahead and get cleaned up while we are in here, or we should probably use the toilet while we are in here.
Remember, visual cues become very helpful as the disease progresses. Showing them what you want them to do and saying the words will help them process what you want them to do.
The incorrect Alzheimer’s approach is the number one cause of resisting care and agitation!
Save yourself from frustration by adding these simple steps to your daily routine. You will be so glad you did!
The Dementia Caregiver Blog Library
Activities, Advanced Directives, Agitation, Apathy, Approach, Apps for Caregivers, Basic Caregiving, Bathing, Bathroom Safety, Caregiver Burnout, Caregiver Compassion, Caregiver Emotions, Caregiver Help, Caregiver Loneliness, Caregiver Support, Cold & Flu Season, Communication Challenges, Dehydration, Dementia Complications, Dementia Doctors, Dementia Safety Home, Dementia Types, Dementia-Friendly, Dressing Issues, Driving Safety, Eating Problems, Fall Prevention, Family Help, Finances, Guns & Dementia, Harm Prevention, Healthcare, Help at Home, Hiding Dementia, Holidays, Hospice, Hospital Stay, In-Between Stage, Kitchen Safety, Laughter, Legal Healthcare, Marijuana use, Medication Tips, Music, Nutrition, Pain, Patience, Poop Problems, Relationships, Reminiscing, Routine, Safety, Sense of Purpose, Shadowing, Sleep Issues, Stages of Dementia, Sundowning, Television, Time Travel, Traveling, Toileting, Wandering
Exploring Caregiving Tools & Resources? Don't Forget to Check Out My Resource Page! 🌟

Hi, I’m Larea, a Certified Dementia Specialist and Registered Nurse with 30 years of hands-on experience helping dementia patients in various settings, from hospitals to nursing homes and hospice. Drawing on personal experiences with my family members and patients over the years, I’m here to help guide you on your caregiving journey.

0 Comments