What is Alzheimers Hospice?
If you are an Alzheimer’s caregiver and have spent time in online groups, you have probably seen talk about Alzheimer’s Hospice. But unfortunately, most people have little or no experience with Hospice, let alone Alzheimer’s Hospice. This post will help clarify Hospice for you, including the who, what, when, where, why, and how of Hospice.
The Hospice concept has been around since the 11th century. It began as a place of hospitality for the sick and dying travelers and pilgrims. In 1967, Dr. Cicely Saunders ( a nurse turned doctor) started the first Hospice in London.
This Hospice focused on comfort care instead of treatment to cure.
Soon after this, several medical professionals began to focus on death. As a result, end-of-life care soon included the patient’s right to choose if they wanted to die at home and focused on death with dignity.

The philosophy of most hospice companies is to treat the person and not the disease and focuses on the quality of life.
You may hear the term comfort care, usually in a hospital setting. Comfort care simply means letting nature take its course with no further aggressive treatment.
Aggressive treatment can be confusing for some people. But, for a cancer patient, it means no more chemo or radiation. It can also mean no more trips to the emergency room. It also means no surgeries, feeding tubes, or continuing aggressive medical regimes that may no longer be helpful or desired.
Hospice levels of care
Routine Hospice Care at home
Continuous Hospice care
Respite Hospice Care
General Inpatient Hospice Care
Where are the Alzheimer’s Hospice levels of care?
- Routine Hospice goes wherever the patient calls home. Whether in a skilled nursing facility, assisted living facility, memory care, or your own home.
- Continuous Hospice care is also known as crisis care provided wherever they are. For example, a medical problem needs a nurse to stay in the home around the clock for a brief time, with a minimum of 8 hours.
- Respite Hospice Care is short-term care (5 days or less) in a nursing home to provide the caregivers at home a break
- General Inpatient Hospice Care is in a hospital setting. Symptoms are no longer manageable at home. They return home when the symptoms are under control.

Who qualifies for Alzheimer’s Hospice?
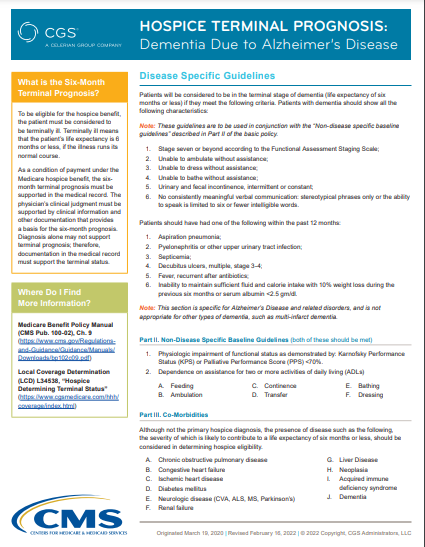
Centers for Medicare & Medicaid Services set the guideline criteria for Hospice care. In addition, there is Dementia due to Alzheimer’s section with the criteria specifics written out.
The first requirement for all patient types in the Hospice guideline is the patient should have a life expectancy of 6 months or less without aggressive treatment.
The Dementia criteria
- Part 1. They must be seven or above on the Functional Assessment Staging (FAST) scale and have one of the listed medical conditions in the prior twelve months.
- Part 2. They must score appropriately on the Karnofsky Performance Scale and the Palliative Performance scale (PPS)
- Part 3. They should have at least 1 of the ten co-morbid diseases listed.
When is it time for Alzheimer’s Hospice?
The life expectancy for someone with Alzheimer’s varies greatly. The average is 4-8 years, but they can live for as long as 20 years. It is time for Hospice when they meet the criteria and are no longer seeking aggressive treatment.
Most people with Alzheimer’s die from complications such as pneumonia, dehydration, malnutrition, falls, pressure injuries, or other infections. At some point, you will run into some of these issues. When you decide to let nature take its course and no longer want medical interventions, it is time to call Hospice.
Hospice is about quality of life, not quantity of life.

How long can they stay in Hospice?
Hospice guidelines require a re-evaluation 90 days after admission and then every 60 days. Therefore, a physician or a nurse practitioner must re-assess them to ensure they still meet the criteria.
They can be discharged from Hospice care if they no longer meet the criteria.
Who pays for Hospice?
Medicare, Medicaid, private insurance, charities, individuals, or other payment programs pay for the hospice costs. Therefore, it is a benefit available to everyone.
What does Hospice provide?
The guideline requires an RN to see the patient every 14 days. There are no other requirements regarding staff. Most hospice companies provide a nurse assistant to help bathe the patients, a social worker, and a chaplain.
The Hospice covers medications related to the hospice diagnosis, but be aware once medicare starts paying the hospice company, they will no longer pay for prescriptions. So when talking with a Hospice company, review what medications they will cover for your loved one.
Necessary equipment and supplies are provided by the Hospice company also. They will even bring incontinent and wound supplies.
Bereavement
One benefit of Hospice many people don’t realize is available would be the Bereavement follow-up. The Medicare guidelines require the Hospice company to provide 13 months of bereavement care to the family after their loved one passes.
Hospice is a great benefit, especially for someone with Alzheimer’s. It provides much-needed assistance to the caregiver and adds a whole team of people to help.
If you have a loved one with Alzheimer’s and aren’t sure if they meet the Hospice criteria, look at the links I provided with the underlined words. Of course, you can always call a hospice company to come and evaluate your loved one if you are unsure or believe they may meet the criteria.

Shelter of Calm:
Your Guide Through Dementia's Storm!
Is Dementia's chaos stealing your peace?
We're here to restore the calm, empowering you to confidently face each challenge.
Take the first step towards transformation now.

The Dementia Caregiver Blog Library
Activities, Advanced Directives, Agitation, Apathy, Approach, Apps for Caregivers, Basic Caregiving, Bathing, Bathroom Safety, Caregiver Burnout, Caregiver Compassion, Caregiver Emotions, Caregiver Help, Caregiver Loneliness, Caregiver Support, Cold & Flu Season, Communication Challenges, Dehydration, Dementia Complications, Dementia Doctors, Dementia Safety Home, Dementia Types, Dementia-Friendly, Dressing Issues, Driving Safety, Eating Problems, Fall Prevention, Family Help, Finances, Guns & Dementia, Harm Prevention, Healthcare, Help at Home, Hiding Dementia, Holidays, Hospice, Hospital Stay, In-Between Stage, Kitchen Safety, Laughter, Legal Healthcare, Marijuana use, Medication Tips, Music, Nutrition, Pain, Patience, Poop Problems, Relationships, Reminiscing, Routine, Safety, Sense of Purpose, Shadowing, Sleep Issues, Stages of Dementia, Sundowning, Television, Time Travel, Traveling, Toileting, Wandering
Exploring Caregiving Tools & Resources? Don't Forget to Check Out My Resource Page! 🌟

Hi, I’m Larea, a Certified Dementia Specialist and Registered Nurse with 30 years of hands-on experience helping dementia patients in various settings, from hospitals to nursing homes and hospice. Drawing on personal experiences with my family members and patients over the years, I’m here to help guide you on your caregiving journey.


0 Comments