Alzheimer’s Dementia Toileting Concerns
Managing Alzheimer’s Dementia toileting Issues in your home can be very difficult. For most people, Alzheimer’s toileting problems usually begin in the middle stage. But, soon, the “accidents” will start.
The first rule is always to stay calm when this happens. Next, remember they will be embarrassed.
Incontinence
Bladder control will go first, and bowel control loss is usually much later. In the medical world, we refer to this as incontinence. Incontinence is the term used to describe the inability to control the bowel or bladder.
As they progress through this illness, their needs will change. Alzheimer’s toileting issues appear when they begin having the occasional bladder accident. Next, they begin to have trouble finding the bathroom. Third, they begin to have problems removing their clothes to go to the toilet.
Eventually, they will fail to recognize the need for toilets. At some point in the late stage, they fail to realize when their bowels or bladder move.

An Alzheimer’s Dementia Toileting routine will help
Beginning an Alzheimer’s toileting routine should be started early on in the disease. Toileting the first thing in the morning, every two hours during the day, and at bedtime is a regular Alzheimer’s toileting routine. Later, they will reach a point when they don’t realize they need to go to the bathroom. Often, a schedule will help you get them to the toilet before they have an incontinent episode.
It is essential to remember keeping to a toileting routine helps prevent accidents!
Watch for signs they need to go to the toilet because they won’t be able to interpret the bladder/bowel signals correctly. For example, pulling at their clothing, wandering around the room, or becoming fidgety may signal they feel the need to void. They are uncomfortable, but they don’t know why they are feeling uncomfortable or what to do to fix it.

Plan for accidents
Understanding how the disease progresses and knowing what to expect next will help. Also, recognizing that incontinence is part of the Alzheimer’s dementia toileting process will help with the frustration of cleaning up an incontinence mess.
Planning for accidents can also help prevent some of the embarrassment that goes along with it. Especially in the middle stage while you are still getting out and going places with your loved one.
Having an extra pair of pants on hand when you go out is an excellent way to prepare for those unexpected accidents. I recommend a bag with pants, underwear or pull-ups, and wipes for the cleanup. Please keep it in your car for emergencies.

Products for Alzheimer’s Dementia Toileting
At some point, you will need to use incontinent products. There are many brands on the market, but there are five main types of products.
The first are the four designed for direct contact with the body.
Male Urine Guard
A protective pouch for men that slips onto the end of the penis to capture urine dribbles. It fits in the front of men’s underwear and discreetly catches urine. Then, they wick away urine to keep the skin dry and comfortable.
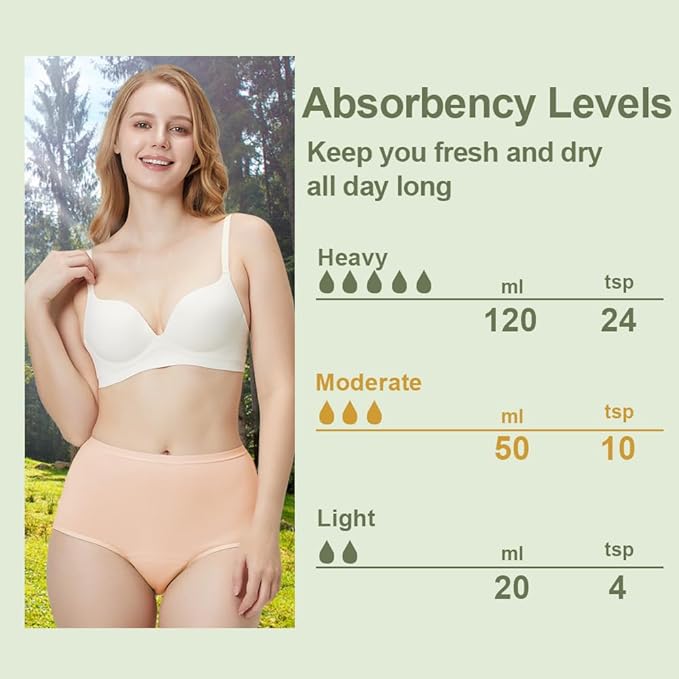
Bladder pads for women
Fitting right into their underwear is similar to sanitary napkins. Many women with different types of incontinence wear these pads. Generally, they can catch urine from a leaky bladder but not a total amount of voided urine.
Pull-up briefs
Look like underwear and are easy to pull up and down. Companies have come a long way with these products. They now have colors and look more like regular underwear. Men are more compliant with gray pull-ups. Women will often wear peach-colored ones or ones with flowers rather than plain white pull-ups. Pull-up briefs are most appropriate for someone who can still get around the house.
Adult diapers
People who are bed/chair-ridden are suitable for adult diapers. Getting them on and off someone who can not stand or help you with the process is much easier. Adult diapers are similar to diapers for children. Tape tabs or Velcro-like material fasten in the front; therefore, they are easier to remove when soiled because they have an area you can tear if needed.
I have added pictures and links to Amazon if you need them.
Male Urine Guard

Women’s Bladder Pad
Pull-up
Adult Diaper
Carewell is a favorite for many caregivers. They carry all of the incontinent supplies and can be set up on auto-ship. Click Here to visit their site
Reusable Incontinence Underwear for Men & Women
Reusable incontinence underwear works well for some people. The underwear is thick and usually absorbs up to 20 ounces of urine for women and 10 ounces for men. These work well for those with Dementia who will not wear Depends.
Reusables also work well for those still able to get out of the house to help prevent an embarrassing accident. However, reusables may be better if you are on a tight budget.
Condom Catheters are also known as Texas Catheters
The condom catheter can be worn with a leg bag during the daytime, especially if the man is still active. The gravity bag is for use at night. Since worn on the outside of the body, there is less chance of infection. In addition, they are effortless to use. Nursing has been using them for many years.
A condom-like apparatus attaches to the penis before connecting it to a drainage bag.
It is attached to a tube connected to a urine collection device. Collection devices are rinsed out and reused. Condom catheters come in different sizes and usually have a sticky area to help secure them. A condom cath helps prevent waking to a soaked morning bed.
Alzheimer’s Dementia Toileting & Cleanliness Concerns
When the loss of bladder begins, you will need to take extra measures to keep the private area clean. It is essential to help maintain cleanliness during this part of the Alzheimers toileting process.
Keeping this area clean will help prevent odors and skin irritation. Also, disposable wipes are the easiest to use.
Watch out for reddened areas. Skin can become irritated, and the skin can break down. Frequently the skin breakdown leads to pressure injuries, also known as bed sores. If you find a reddened area, you can treat it before it becomes an open area.
Assisting with toileting care can be awkward for both of you.
Everyone does this in private, and as your loved one progress in the disease, they will begin to resist toileting more. Gentler reminders are often the easiest once the incontinence stage begins.
Resisting Toileting
Towards the late stage, you will need to change your tactics as they begin to resist toileting. Toileting and bathing become dreaded tasks. Eventually, those become words they don’t like to hear. I share a few tips to help with that in my Approach Blog.
I recommend investing in a waterproof mattress cover. It is rare for a person with middle or Late-stage Alzheimer’s Disease to make it through the night without wetting.
Alzheimer’s Dementia Toileting and Fluid Intake
Cutting back on fluids later in the evening can decrease urine output at night. However, if you cut back on liquids during the evening, ensure they still get plenty of fluids during the day. Lack of fluids can lead to dehydration, which can lead to serious medical problems.
All kinds of products are on the market to help you manage incontinence products at home. For example, cloth and disposable bed pads fit in the middle of the bed to catch urine, which can be used along with pull-ups or Depends to make cleanup easier.
The 5th type of incontinent products are the under-pads to be used on the bed or in chairs when they are up.

Incontinence Pads
Incontinence Pads are a necessity for late-stage Alzheimers toileting issues. Creating a waterproof moisture barrier between any liquid and furniture is essential. They can be placed on a chair or bed to prevent leaks from ruining the furniture. They have disposable and cloth pads available.
Paper pads such as the hospital’s use can be disposed of when they get soiled. Unfortunately, both types of padding tend to roll up or wrinkle easily.
Remember to check for wrinkles. A wrinkle left under someone can cause their skin to break down.
These are the reusable pads. These come in different sizes but I prefer this larger size.
Make sure the toilet is accessible and safe
As the disease progresses, they will have trouble finding the bathroom. Therefore, keeping the path to the bathroom clear and well-lit is best. Some people have found that placing a picture of a toilet on the door will help serve as a reminder.
Make sure it is easy for them to get on and off the toilet. Grab bars on the wall to help can make a big difference. So can a raised seat. My preference has always been a bedside commode with arms. Removing the commode bucket, allowing the commode to fit right over the toilet. The commode is taller than the toilet and raises the seat, giving them handrails to hold onto, and it can be used at night by the bed if needed. The bedside commode is also the safest to use.
Bowel Issues and Alzheimer’s Dementia Toileting
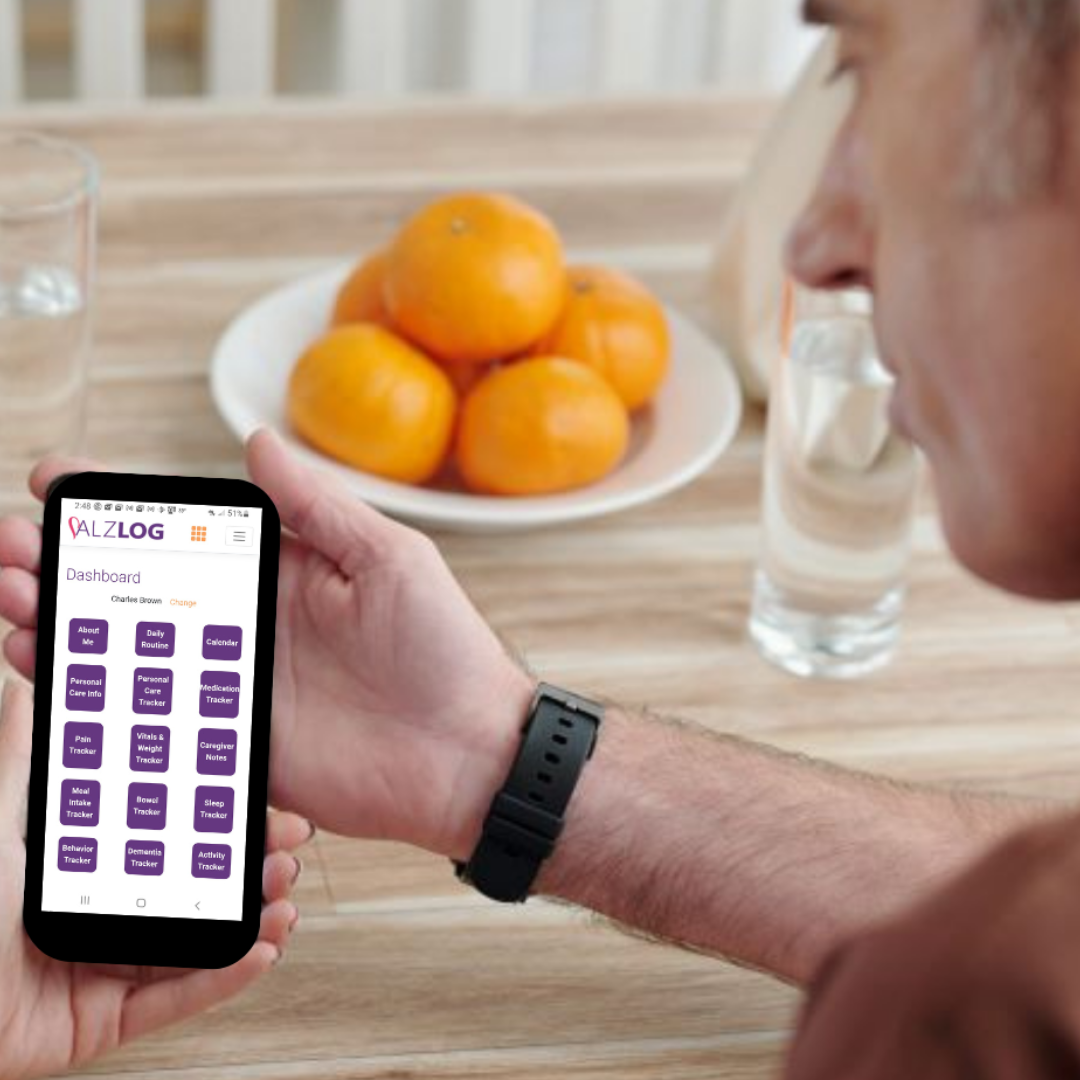
Taking care of toileting needs is crucial in dementia care. Tracking bowel movements using an app like Alzlog can be a real game-changer, especially in the middle to late stages. This helps in preventing problems like constipation and impactions.
It’s generally recommended that bowels should move at least every three days to steer clear of complications. Having a chat with your doctor about bowel protocol and preferred interventions is a smart move.
Make sure to have a well-thought-out bowel plan in place. And for more detailed insights into managing poop issues related to dementia, head over to my page specifically dedicated to that topic.
Remember: for all of Alzheimer’s Dementia toileting issues, it’s always good to stay proactive and informed!
The Dementia Caregiver Blog Library
Activities, Advanced Directives, Agitation, Apathy, Approach, Apps for Caregivers, Basic Caregiving, Bathing, Bathroom Safety, Caregiver Burnout, Caregiver Compassion, Caregiver Emotions, Caregiver Help, Caregiver Loneliness, Caregiver Support, Cold & Flu Season, Communication Challenges, Dehydration, Dementia Complications, Dementia Doctors, Dementia Safety Home, Dementia Types, Dementia-Friendly, Dressing Issues, Driving Safety, Eating Problems, Fall Prevention, Family Help, Finances, Guns & Dementia, Harm Prevention, Healthcare, Help at Home, Hiding Dementia, Holidays, Hospice, Hospital Stay, In-Between Stage, Kitchen Safety, Laughter, Legal Healthcare, Marijuana use, Medication Tips, Music, Nutrition, Pain, Patience, Poop Problems, Relationships, Reminiscing, Routine, Safety, Sense of Purpose, Shadowing, Sleep Issues, Stages of Dementia, Sundowning, Television, Time Travel, Traveling, Toileting, Wandering
Exploring Caregiving Tools & Resources? Don't Forget to Check Out My Resource Page! 🌟

Hi, I’m Larea, a Certified Dementia Specialist and Registered Nurse with 30 years of hands-on experience helping dementia patients in various settings, from hospitals to nursing homes and hospice. Drawing on personal experiences with my family members and patients over the years, I’m here to help guide you on your caregiving journey.













0 Comments